Many people in their lifetime experience a sudden feeling of dizziness, be it head spinning, light-headedness, a floating sensation or a loss of balance, sometimes associated with nausea. In fact, dizziness is a frequent complaint.
It is estimated 30% of the general population have experienced moderate to severe dizziness at least once in their lifetime, and nearly 2% of adults seek medical attention annually for a new symptom of moderate to severe dizziness or vertigo.
The prevalence of symptoms of dizziness is particularly high among older people, with between 10% and 30% thought to suffer. Dizziness can be extremely distressing and physically debilitating and can markedly impair quality of life. In older people, in particular, experiencing dizziness makes the sufferer twice as likely to report disability, worsening of depressive symptoms, reduced participation in social activities, poor health and falls.
People generally find it hard to describe their dizziness symptoms and use vague terms such as floating, spinning, unsteadiness and giddiness. This imprecise symptom description is a major reason why dizziness is complex to assess and treat.
Doctors describe it as a feeling of altered orientation in space and classify it into four main subtypes:
- unsteadiness caused by leg weakness and impaired sensation
- dizziness from severe anxiety
- light-headedness
- vertigo
Why do we feel dizzy?
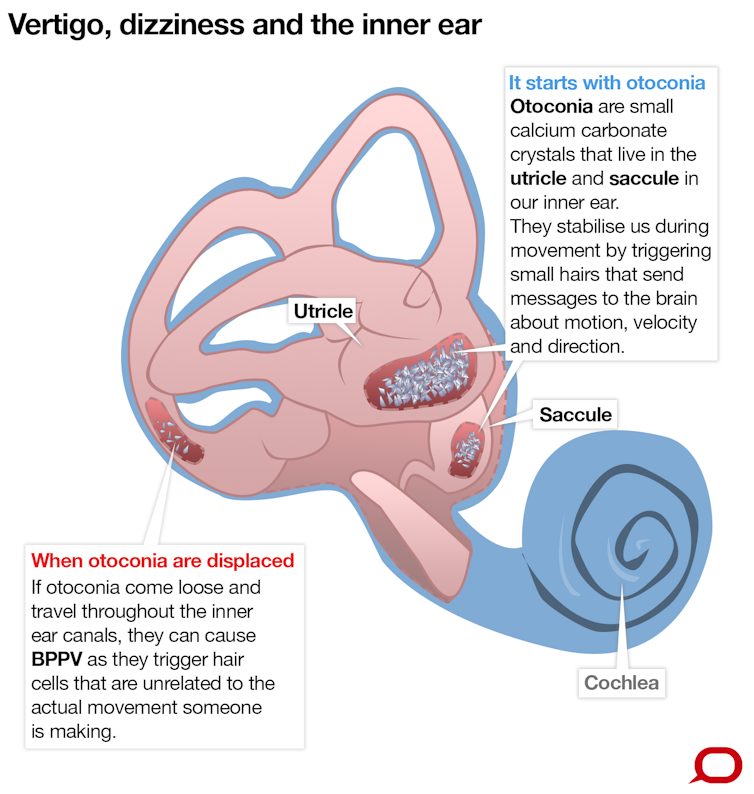
Vertigo is diagnosed when patients express having the illusion of head or body spinning. Vertigo tends to be caused by the inner ear (vestibular) - most commonly by the displacement of calcium crystals (small stones in the inner ear whose movement informs the eyes and the brain of horizontal or vertical movements) from their correct chambers in the inner ear – a condition called Benign Paroxysmal Positional Vertigo or BPPV.
As the calcium crystals blunder their way through one of the three inner ear canals, they activate very thin nerve cells (known as hair cells) connected to the brain and the eyes. The hair cells are highly sensitive to any slight movement and their signals to the brain normally reflect head movements and enable eye movements and body posture to be instantly adjusted.
In BPPV, the hair cells incorrectly inform the brain of head movement. This differs from the information provided by the eyes causing disorienting head movement or dizziness. Closing the eyes removes one of the disagreeing sensory inputs and the dizziness subsides.
Similar feelings of head spinning can also be caused by other inner ear conditions, including vestibular nerve or inner ear infections (neuritis) or blocked vestibular canals, affecting the nervous pathway (called a “reflex”) that links the inner ear and the eyes.
The role of this reflex is to keep stable and clear vision when the head is moving, especially at fast speeds, for instance when walking quickly, running or even sitting in a car on a bumpy road. If this reflex isn’t functioning properly, vision is like watching the world as it appears on a poor quality homemade video: shaky and unstable.
Almost as frequent is the feeling of light-headedness people experience when getting up after lying on the couch or a bed quickly or from standing up from a chair after sitting for a long time.
In this instance, blood has pooled in our legs and the heart does not increase its beating rate sufficiently to compensate for the increase in blood pressure needed for standing up. This inadequate blood pressure regulation results in too long a time lag for providing the brain with oxygenated blood and dizziness occurs.
How to treat dizziness
Treatments for dizziness include physical manoeuvres such as moving the crystals back into their chamber for BPPV, blood pressure medication management and balance training. Many middle-aged and older sufferers, however, often find it hard to receive a correct diagnosis and are unable to gain relief from their symptoms.
This may be due to the unavailability of diagnostic tests for some inner ear conditions, the off-and-on nature of the problem making it hard to pinpoint, more than one issue leading to the problem and health care providers being only being able to diagnose one or two of several possible causes.
At NeuRA we are completing a study evaluating a one-stop assessment and treatment for dizziness. If successful in reducing dizziness episodes and handicap, we hope to make this strategy available for incorporating in clinical services.

